MCO
Understanding MCO's & Where they fit into waiver services
A Managed Care Organization (MCO) is a healthcare delivery system designed to provide coordinated, cost-effective care to individuals. MCOs focus on integrating preventive, primary, and specialty care to improve health outcomes while managing costs. They are a key component of the American healthcare system and play an essential role in Virginia Medicaid.
Care Coordinator: Each MCO assigns a Care Coordinator to support and manage a member’s healthcare needs. The Care Coordinator serves as the primary point of contact for the member and their family. Their responsibilities include:
Acting as your main contact for any questions about healthcare services.
Working with you to develop a written plan that addresses your health needs.
Arranging transportation to and from medical appointments when needed.
Providing interpretation services to support communication if necessary.
Ensuring you have all required pre-approvals and referrals for medical services.
Managed Care Organizations are critical to the Medicaid system, as they strive to ensure members receive high-quality, timely care while also controlling healthcare costs. They influence how services are delivered and how members interact with healthcare providers, ultimately impacting health outcomes and overall satisfaction with care.
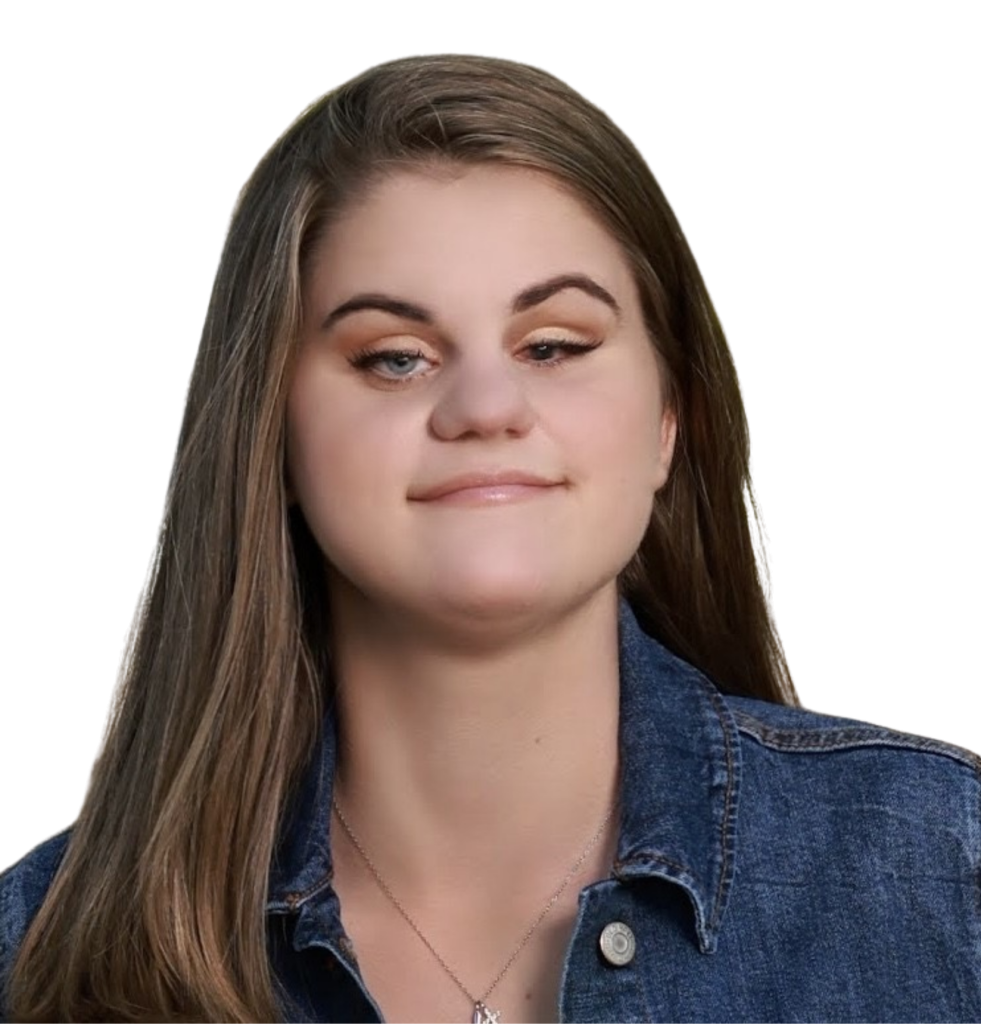
Meet Kim, Age 23
Kim is a 23-year-old young woman with an incredible spirit. Despite managing multiple diagnoses, including blindness, epilepsy, autism, mild cerebral palsy, hydrocephalus, and anxiety, she continues to shine brightly in everything she does. Kim approaches life with determination, resilience, and grace. Her positivity and strength inspire everyone who knows her, proving each day that she is truly unstoppable and absolutely fabulous.
MCO Contact List
Aetna Better Health (VA CCC Plus & FAMIS)
- CCC Plus Member Services & Language Interpretation & Transportation: 855‑652‑8249
- Medicaid/FAMIS Member Services: 800‑279‑1878
Anthem HealthKeepers Plus
- Member Services (FAMIS/Cardinal Care): 800‑901‑0020
- Language Interpretation: 855-323-4687
- Transportation (Access2Care): 877‑892‑3988
Humana Healthy Horizons
- Member Services & Language Interpretation: 1‑800‑424‑4524
Sentara Health Plan (Optima/Sentara Medicaid)
- Member Services: 757‑552‑7401 or toll‑free 877‑552‑7401
- Language Interpretation: 855-687-6260
UnitedHealthcare Community Plan
- Member Services: 844‑368‑7151
- Language Interpretation: 800‑789‑8050
- Transportation: Contact Member Services or refer to ID card
How MCOs Help You
Your MCO is here to support you in many areas of your care, including:
- Coordinating your care and services
- Approving hours for waiver services
- Providing access to Medicaid-covered healthcare
- Connecting you with a dedicated Care Coordinator
- Assisting with appeals or grievances if issues arise
MCOs play a central role in your Medicaid coverage. By working closely with your Care Coordinator and understanding your benefits, you can get the most out of
the services available to you.
What is a Managed Care Organization (MCO)?
A Managed Care Organization (MCO) is a healthcare system designed to provide coordinated, cost-effective care, with a focus on prevention, primary care, and access to specialists. MCOs are a key part of the Virginia Medicaid Waiver system and play a major role in how services are delivered and managed.
“From Toddlers to Grandparents, we’re here to walk beside you with care, dignity, and personalized support.”

What to Expect

Access to Medical Benefits